It’s Movember—and the PSA debate is back. After 23 years of follow-up, the ERSPC now provides in the NEJM the strongest numbers to date: 2 fewer deaths and 27 more overdiagnoses per 1,000 screening invitations. Here’s everything you need to know for patient conversations.
Urologists, family doctors and researchers have battled over PSA screening for decades. Now, after remarkable 23 years of follow-up, the landmark European Study of Prostate Cancer Screening (ERSPC) got published in the NEJM. It won’t settle the debate, but it gives us credible numbers to have honest conversations with patients. Let’s dive in!
Why does it matter?
Prostate cancer is everywhere. It’s the most common cancer in men and even found in 59% of men over 80 at autopsy. Yet only 1 in 27 men die from it. This paradox is the central screening challenge: it’s usually benign, but sometimes deadly. PSA can’t tell the difference.
What’s the ERSPC Study?
A randomized trial of 160,000 men from 8 European countries:
- Median age was 60 years at randomization (55 to 69 years)
- Median follow-up was 23 years (21 years considering deaths)
Intervention group:
- Invitations mainly every four years
- Men performed two PSA tests on average
Control group:
- Not invited for screening
- We don’t know how many PSA tests they performed nevertheless
ERSPC: What were the key results?
Per 1,000 invited men:
- Benefits: 2 fewer deaths over 23 years
- Harms: 27 excess diagnoses -> anxiety, biopsy, surgery, erectile dysfunction
But real benefits might be larger (it didn’t test getting but being invited to PSA tests) and harms might be lower (because of new and improved treatment options and standards).
What were the benefits of being invited to a PSA-Screening?
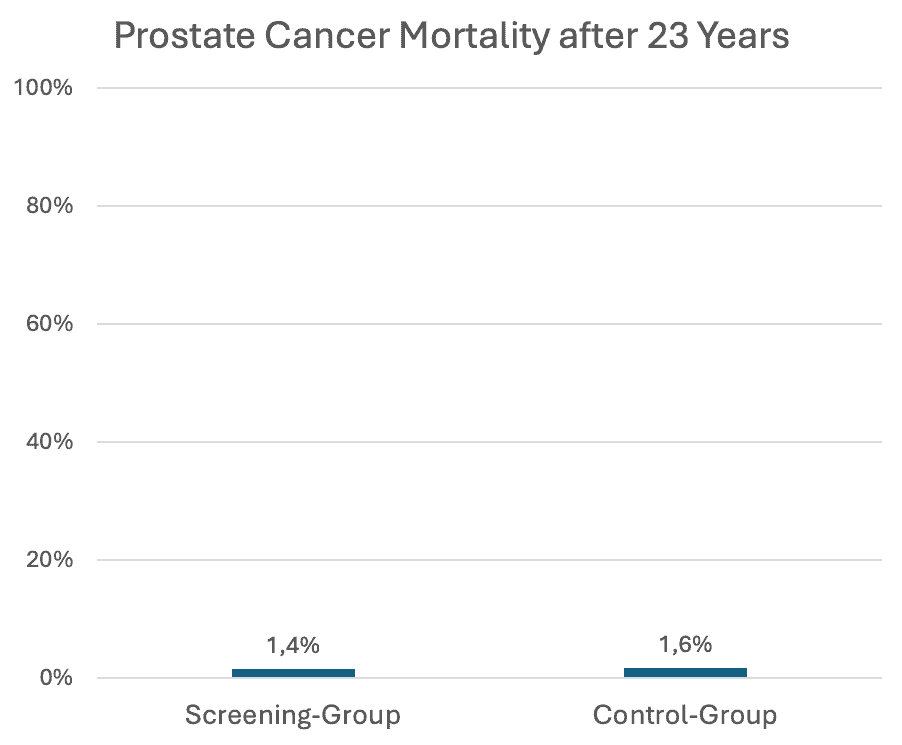
What does this graph mean? Here is the same result presented by four different numbers – to show you the power of risk communication:
- 22% less prostate cancer deaths (Absolute Risk Reduction, ARR)
- 2 deaths were avoided per 1,000 men being invited (Absolute Risk Reduction, ARR)
- 456 men needed to be invited to avoid one death (Number Needed to be Invited for Screening, NNIS)
- 13% lower prostate cancer mortality (Relative Risk Reduction, RRR)
The two other major randomized trials of PSA screening (JAMA 2024 and AIM 2017) confirm this result. The observed mortality reduction is most likely real, but small.
What were the harms of being invited to a PSA-Screening?
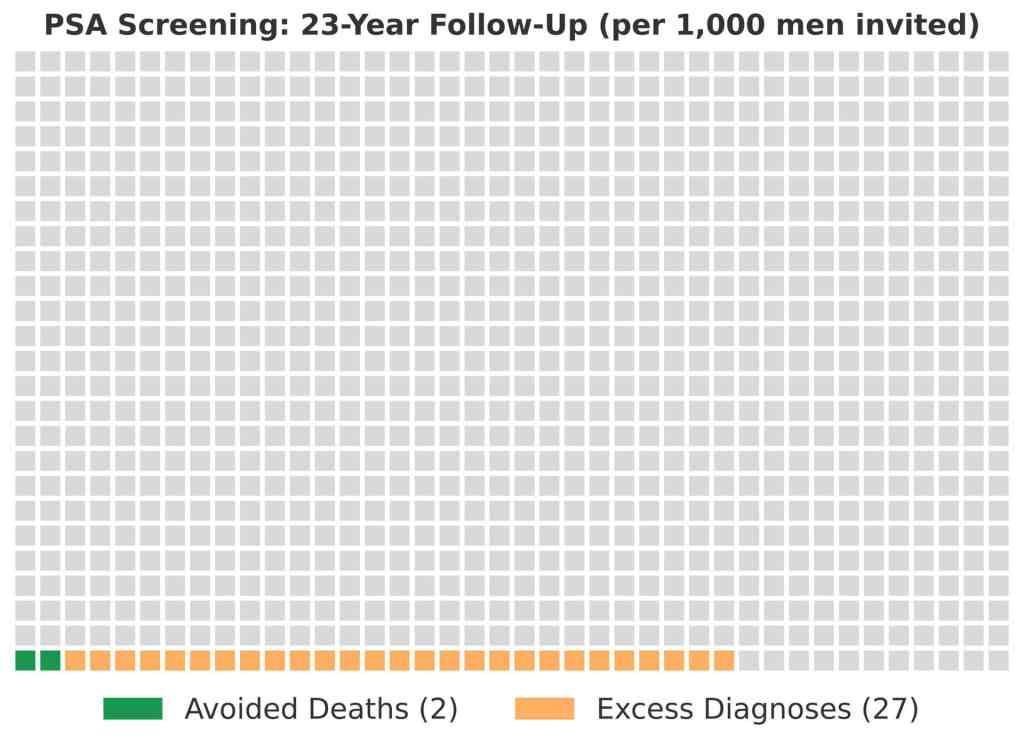
This graph shows that for ever 1,000 men invited to PSA screening, two deaths were avoided, and 27 other men were overdiagnosed with prostate cancer. In the same time period, half of all men died from other causes.
“Healthcare providers need to know how to represent information so that their patients can actually understand what it means.”
(Gerd Gigerenzer, advocate of natural frequencies for risk communication)
Why is an excess diagnosis harmful?
- Elevated PSA can lead to anxiety and follow-up visits.
- Elevated PSA often leads to a biopsy. Bleeding, infections and urinary retention are possible complications.
- A positive biopsy often leads to surgery or radiotherapy, which can cause erectile dysfunction, urinary or faecal leakage (see my article here).
Why does this trial not reflect clinical practice in 2025?
Benefits are (probably) larger:
- The study only tested being invited to PSA tests, not taking
- The control group likely received PSA tests too.
- Participants only received two PSA tests (on average).
- Men were already 60 years old at randomization (mean).
Harms are (probably) lower in 2025:
- 89% received a biopsy after an elevated PSA test. Today, you retest and do an MRI scan
- Active monitoring became more common (see my article here).
- Surgery became more nerve-sparing and higher volumes are required.
What do Guidelines recommend?
While all major guidelines agree to recommend PAP smear, mammography, colonoscopy and lung scans, and agree to not recommend ovarian and thyroid cancer screening, PSA screening is the great exception. Here’s their disagreement:
- Offer PSA tests only after shared decision making, usually every 2-4 years between age 50-69 for men at average risk: European Association of Urology, American Urological Association and Choosing Wisely
- Offer PSA tests only after request by the patient, don’t raise the issue proactively: NICE (UK)
- Don’t offer PSA tests: CDC/USPSTF, AAFP, Canadian Task Force
This NEJM 23-year Update perfectly explains why these guidelines don’t agree, and why no single country implemented a national PSA screening program. Decisions remain complicated and individualized. Groups like urologists (EAU, AUA) see cancer mortality and believe in modern technology, and groups like family doctors (AAFP, CTF) see overdiagnosis and its long-term harm.
“We must be honest about what we know, what we don’t know,
and what we simply believe.”
(Otis Brawley, Chief Scientific Officer of the American Cancer Society)
Key Takeaways for Your Patients
- Shared Decision Making is Still Crucial. This study doesn’t offer a simple “yes” or “no” either. But it gives us the numbers to have better conversations.
- Quantify the Discussion. “If we invite 1,000 men to regular PSA tests, we can save 2 lives and find 27 extra cancers. Some of them will get unnecessary treatment and complications.”
- Context is Important. We should also tell them that benefits might be larger, and harms smaller. Due to study flaws and medical advances.
- Stop Screening the Young/Elderly/Unwell. Even major Urological Associations (EAU, AUA) don’t recommend routine PSA-screening of men at normal risk before 50 years, after 70 years, or with a life expectancy of less than 15 years. Unfortunately, testing rates are still three times higher in patients in their 70s and 80s (in the UK).
- Apply the Teach-Back Method. It’s simple, quick, and improves patient understanding and recall. Read more here.