As early as 1897, Hill and Barnard called for standardization of blood pressure measurements, since arm position affects the results (see BMJ 1897). Yet, a review in 2014 showed that guidelines and studies still recommend and use different arm positions. So, here is a “standard”…
What do the current ESC guidelines from 2024 recommend?
- Sit comfortably for 5 minutes.
- Rest your arm on a table (to avoid isometric strain).
- Expose your upper arm (avoid rolling up sleeves due to cuff obstruction).
- Use a validated device with the correct cuff size (only 6% of devices were adequately validated).
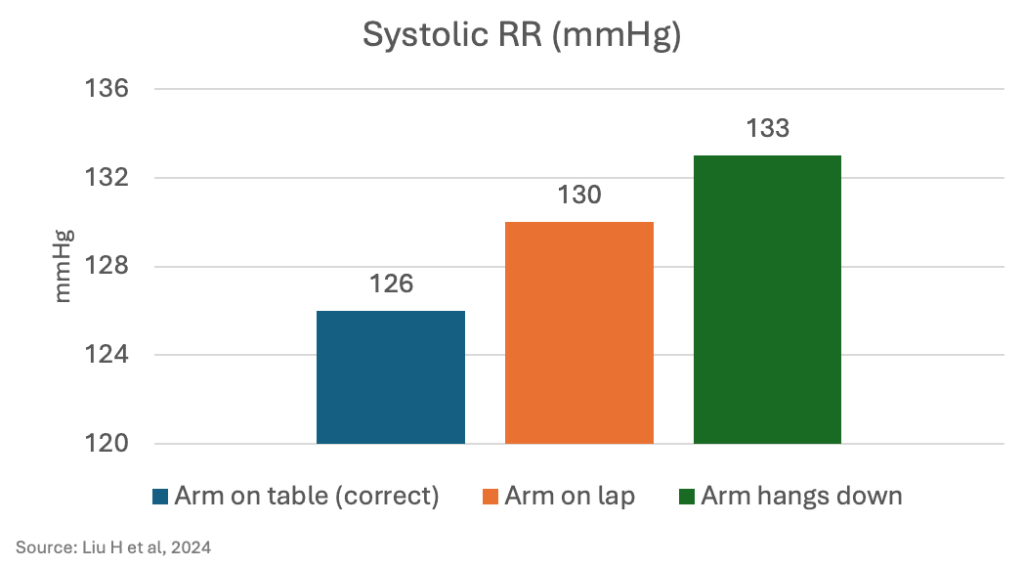
How important is the correct arm position?
A randomized study published in October 2024 tested three different arm positions with 133 participants (average age 57). The blood pressure readings showed significant differences. A wrong arm position can thus lead to misdiagnoses and over-treatment:
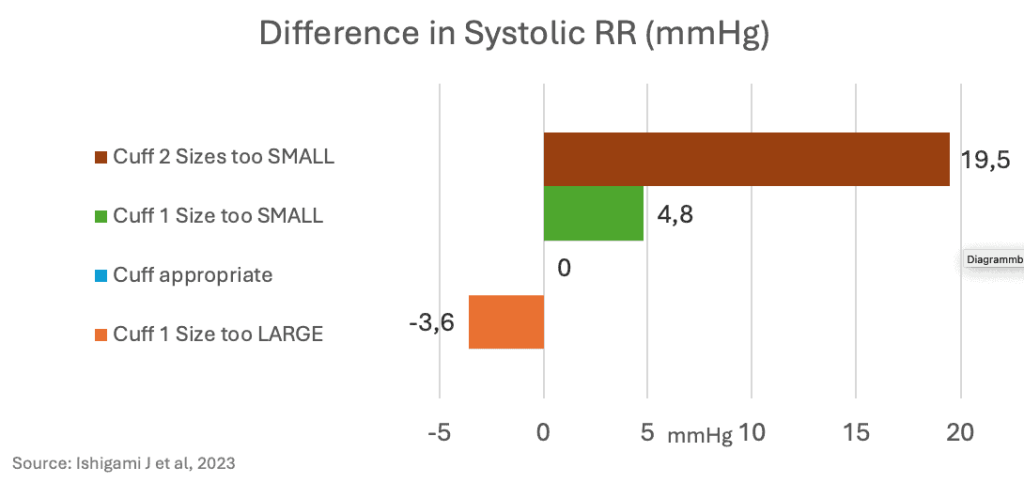
How important is the correct cuff size?
In October 2023, the first randomized study was published, testing different cuff sizes in 195 participants (average age 54). The study found that using the wrong cuff size led to misdiagnoses, particularly when cuffs were too small for obese patients:
Are wrist blood pressure measurements reliable?
A systematic review (BMJ Open 2016) of 20 studies examined the accuracy of blood pressure measurements in obese adults with large upper arm circumferences. It showed that, for these patients, a measurement on the upper arm with the correct cuff size was meaningful. However, if the cuff was too small, wrist measurements (at heart level!) were found to be more accurate, with better sensitivity and specificity. The 2024 ESC guidelines consider wrist measurements (in the office) as a possible alternative.
Are blood pressure measurements by a smartwatch reliable?
Recent observational studies concluded that the accuracy of these measurements was either “insufficient” or “adequate“. More and better studies are needed.
Are home blood pressure self-measurements effective?
Last week (November 21), a systematic review of 65 studies was published. It showed a significant, but small, reduction in blood pressure of 3.3/1.6 mmHg. It remains questionable whether this modest effect is clinically relevant, or whether it justifies the effort and potential worries of patients.
Conclusion:
When measuring blood pressure on the upper arm, it’s important to rest the arm on a table and to use the correct cuff size. For severely obese patients, wrist measurements can be a useful alternative.