A chronically exhausted patient hopefully asks for a high-dose vitamin C infusion. Where does this belief come from, and what does the science say?
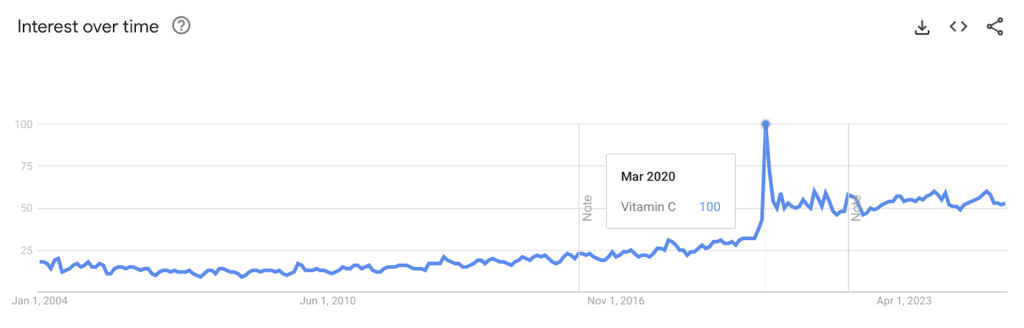
The evidence base is thin. Nevertheless, vitamin C has experienced a remarkable renaissance since the pandemic, as Google search queries show:
This article separates historical myths from evidence-based medicine – and tells a fascinating story in the process.
First, the “hard evidence”
The most studied area is the common cold. The preventive administration of vitamin C was able to slightly reduce the duration and severity of symptoms. A therapeutic administration for existing symptoms was ineffective. Here are the results of the Cochrane Review (56 studies, 11,000 patients, ≥200 mg/day):

Here is a summary of the most relevant evidence (mainly Systematic Reviews and Guidelines) for widely discussed indications:
Indication | State of Evidence | Brief Conclusion |
Fatigue – ME/CFS – Long-COVID | · NICE 2021: no vitamin therapy for ME/CFS · AWMF 2022: vitamin therapy for ‘fatigue’ not even mentioned · Systematic Review 2021: 9 studies, but in cancer and zoster patients, mostly significant effects and severe methodological flawsA good RCT 2012: 141 healthy office workers, small effect (-0.7 points on a 10-point scale) | There are no high-quality studies on vitamin C (p.o./i.v.) for these indications. Fatigue in cancer patients or at work has significantly different pathomechanisms. |
Wound Healing | · Systematic Review 2022: 18 small, heterogeneous studies; most were significant with partly clear effects · Pressure Ulcer RCT (1974!): Wound area reduced by 84% (vitamin C) vs. 43% (Placebo) · Ulcer RCT (2020): Healing at 100% vs. 56% after 8 weeks | The evidence is limited, but shows clear effects in some cases. |
Cancers | · Systematic Review 2025: 3 small studies on colon/stomach CA, not significant · Systematic Review 2019: 19 studies of various cancers, all methodologically very limited · Pankreatic cancer RCT 2024: median survival 16 vs. 8 months with 75g i.v. 3x/week (p=0.03) | There are hardly any high-quality studies on this, despite plausible pathomechanisms (i.v.). |
Iron Absorption | · Two Systematic Reviews (2023) showed no significant or a significant but clinically irrelevant increase in Hb/Ferritin | According to physiology, vitamin C should help with iron absorption. In practice, however, it does (almost) nothing. |
Side Effect: Kidney Stones | · Systematic Review 2019: four studies showed significant effects only at some daily doses in men | According to physiology, vitamin C promotes calcium oxalate stones. Studies only partially confirm this. |
Vitamin C for Fatigue: The History of an Invented Indication
From the disease…
More than 2 million sailors died from scurvy between 1500 and 1800. Although Vasco da Gama learned as early as 1497 that citrus fruits help, this was not experimentally confirmed until 1747. Sir James Lind gave 12 sailors sick with scurvy six different foods. Those given oranges/lemons showed rapid improvement – the first controlled clinical trial in history was born!
…to propaganda.
Vitamin C was discovered in 1912, isolated in 1928, synthesized in 1932, patented in 1934, and honored with two Nobel Prizes in 1937. The company Roche now had a promising product – but the market for scurvy was tiny. That’s why internal documents from 1939 stated:
«The harmless person, especially the housewife, does not ask [sic!] for it; neither tongue nor eye is tempted to buy by the vitamin content. The task was therefore: to create the need in the first place […] through propaganda.»
As a result, vitamin C was produced for dogs and cats, for vitamin-enriched skin creams, nylon stockings, and cigarettes, and even for a new type of explosive.
From the fatigue invention…
The big breakthrough, however, came with the invention of new indications – vitamin C for fatigue, susceptibility to infection, wound healing, and pain. Without any science to back this up. Today, 90 years later, these indications are still popular. At first, however, the pharmaceutical representatives were – unexpectedly – laughed at by General Practitioners. Roche actually thought that the “practical doctors” would have a great interest in vitamin C due to “the public’s belief in vitamins,” in contrast to the “scientifically-minded representatives of the medical profession, i.e., especially clinicians and specialists.” However, they were laughed at by “over 80% of GPs” because it was “a fad that would soon disappear.” (Source)
…to disease mongering.
But the propaganda department did not give up. It planned to define “where the field of C-hypovitaminosis actually begins,” which became a reality with the introduction of a recommended daily dose in the USA in 1941, expanding the market. Furthermore, sports doctors, professional cyclists, and soldiers were identified as multipliers – today we would call them influencers – and supplied with information by Roche’s “scientific service.” During the Second World War, vitamins even became a new civic duty, as contemporary advertising for “Victory Vitamin C” shows:

Roche’s strategy was successful, at the time generating up to three-quarters of its revenue from vitamin C. These tactics – inventing new indications (“off-label”), expanding diagnostic boundaries (“disease mongering“), and recruiting opinion leaders (“influencers”) – still exist today, and we should recognize them.
The Nobel Prize Winner Effect: Hype & Backlash
The story of vitamin C is inextricably linked to one man: Linus Pauling. He was the only person to receive two unshared Nobel Prizes – in Chemistry in 1954 and the Nobel Peace Prize in 1962. A lecture 1960 would change his life and the history of vitamin C forever. A man in the audience, Irwin Stone, subsequently wrote him a letter recommending he take 3g of vitamin C daily to live longer. Pauling felt “more alive and healthier” afterwards, increased his daily doses up to 18g, and became scientifically obsessed with vitamin C.
His book Vitamin C and the Common Cold (1970) became a bestseller due to his fame, and pharmacies reported a 10-fold jump in sales. The scientific community was also enthusiastic, publishing 29 RCTs on the subject in the 1970s. The hype had reached its peak.
However, when three negative studies were published simultaneously in 1975 in JAMA, it quickly came to an end. Although it later became clear that these three studies had serious methodological flaws, the textbook verdict of “no benefit” was sealed. Since then, there have been very few RCTs on the topic and a “cognitive bias” in the medical community – negative studies on vitamins were uncritically accepted, while positive studies were sceptically rejected. Good science, however, should always remain objective.
Scientific Learning Points
- Financial conflicts of interest are relevant. Economically, it made sense to invent new indications, lower thresholds, and use multipliers.
- Anecdotal evidence should never be overestimated. Pauling’s personal experience was likely a placebo effect, or he coincidentally felt better afterwards.
- Eminent figures are also only human, even double Nobel laureates. Pauling was often scientifically correct, yet he could also be wrong.
- Headlines increase sales. A drug’s popularity usually has little to do with the reliability of the evidence.
- Cognitive bias must be avoided. An unjustified hype is just as unscientific as its dogmatic overcorrection.
- For 90 years, we have been debating whether vitamin C helps against fatigue, infections, ulcers, and cancers. The fact that we still lack clear answers is also a weakness in science. Such commonly applied therapies should be studied properly.
Practical Summary for Patient Conversations
- The idea that vitamin C helps with fatigue is 90 years old and is based on a marketing campaign and the personal opinion of a famous Nobel laureate, not on scientific evidence.
- For fatigue, ME/CFS, and Long-COVID, there are no high-quality studies.
- For colds, only daily preventive intake has a (small) effect.
- For pressure sores/ulcers, it could be quite helpful (few, small studies).
- Iron absorption might increase only (a little).
- Natural sources are a good alternative – just 1 pepper, 1 orange, or 1 broccoli contains the recommended daily dose of vitamin C.